What's a 'Normal' A1C? When Is It Misleading?
Key Takeaways:
- A1C is a type of blood glucose test that measures your average blood sugar levels over 2-3 months.
- The A1C test can be a useful measurement for diabetes management and a screening tool to help diagnose prediabetes and diabetes.
- Factors that can misleadingly affect A1C include certain health conditions, pregnancy, and medications.
Hemoglobin A1C (aka HbA1C or just A1C) is the standard for measuring blood sugar in people with diabetes. An A1C test reflects your average glucose levels over two to three months.
Studies have found higher A1C levels are associated with an increased risk of diabetes complications such as heart problems, kidney disease, and diabetic neuropathy (nerve disease). For every 1% decrease in A1C, there is significant protection against those complications.
However, as an average over a period of months, A1C cannot capture critical information such as time in range (70-180 mg/dL) and time below range (less than 70 mg/dL). So, why is A1C used in the first place? Here's what an A1C test is helpful for, as well as factors that can lead to misleadingly high or low values.
What is A1C and why is it used?
A1C is a type of blood test that estimates a person’s average blood sugar levels over two to three months. Since it captures blood glucose levels over a period of time, an A1C test can be a useful tool for diabetes management. A1C can also be used as a screening tool to help diagnose prediabetes and diabetes (elevated A1C levels over time can be an indicator of diabetes).
A1C is usually measured in a lab with routine blood work, or with a countertop machine in a doctor’s office (and some pharmacies) using a fingerstick.
An A1C test measures the relative percentage of what's called “glycated hemoglobin,” which refers to how much hemoglobin (an important component of red blood cells) has sugar attached. If a person consistently has higher blood glucose levels, A1C will go up because more red blood cells are coated with sugar. Once a red blood cell becomes coated with sugar, the link is irreversible; it's only when red blood cells are "recycled" (which happens every two to three months) that the sugar coating disappears.
Though A1C doesn’t provide day-to-day or hour-to-hour information as continuous glucose monitoring (CGM) does, it's still helpful for understanding how well your diabetes treatment plan is working over time.
It can also be helpful for determining your risk of diabetes-related complications. For example, a lower A1C is correlated with a lower risk of microvascular complications, such as kidney disease, vision loss (retinopathy), and nerve damage. Similarly, a consistently high A1C can lead to macrovascular complications like heart disease.
What are “normal” A1C levels?
Generally, a high A1C value indicates high average blood sugar levels – that means you might be at risk for or already have diabetes. Here are the following cutoffs for A1C per the American Diabetes Association:
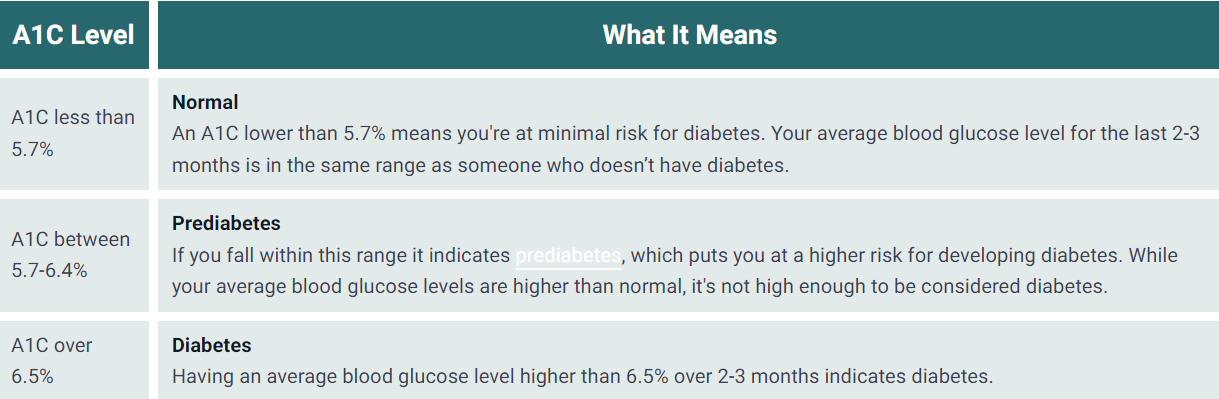
Screening is critical to the prevention or early diagnosis of diabetes; make sure to get an A1C test if you think you might be at risk for diabetes.
For people who have diabetes, an A1C of less than 7% is the goal. Since each person with diabetes is unique, however, healthcare providers are recommended to set individual goals as A1Cs may differ depending on age and other health conditions.
How does age affect A1C?
Where is A1C misleading or potentially inaccurate?
Much progress has been made in standardizing and improving the accuracy of the A1C test thanks to the National Glycohemoglobin Standardization Program (NGSP). Results from a non-NGSP certified lab may not be as reliable.
Depending on the machine, a single A1C test can have up to a 0.5% margin of error, which means the “true” value might be 0.5% higher or lower than the measured A1C. For example, if a lab report shows an A1C value of 7%, the actual A1C value might range from 6.5% to 7.5%.
As mentioned, A1C is based on a person’s red blood cell turnover (the lifespan of a red blood cell) and the quantity of sugar attached to each cell. Many factors can impact A1C and red blood cell turnover including certain conditions (like kidney disease), hemoglobin variants, types of anemia, and certain drugs and vitamins. This can result in misleading A1C values.
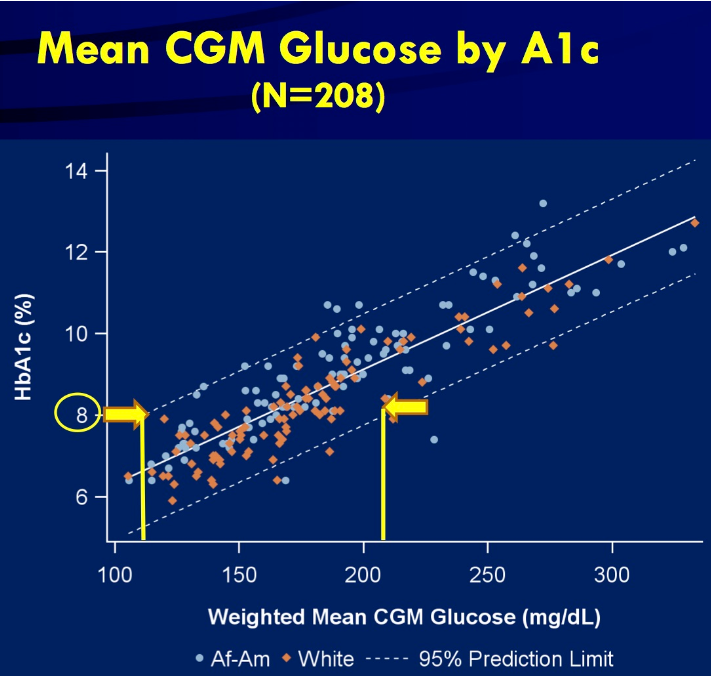
The relationship between A1C values and average blood sugar levels can also vary markedly from person to person. In studies using CGM, 24/7 blood sugar levels can be compared to a measured A1C. These studies reveal considerable variation between participants. For instance, an 8% A1C value in one person could reflect an average blood sugar of 140 mg/dL, while in another it could be 220 mg/dL.
A1C to blood sugar conversion
Calculating A1C to blood sugar, or estimated average glucose (eAG), is done through a mathematical equation. If you know your A1C values you can find out how that translates to blood glucose using a conversion calculator. Results can vary, but here's a quick look:
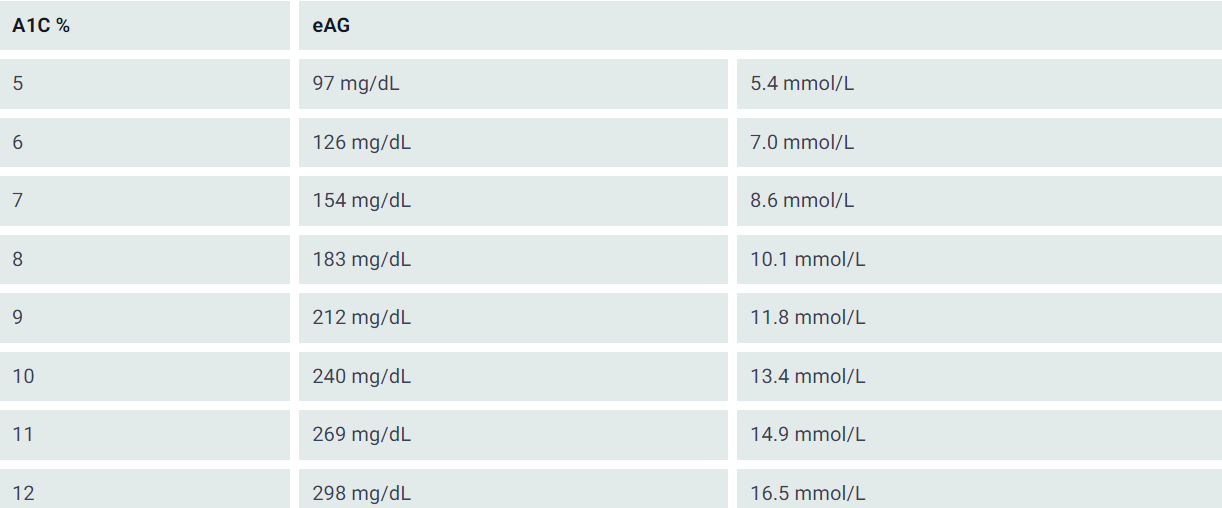
For looking at an individual’s glucose values, CGM is a better tool for measuring average sugar levels, time in range, and time below range.
What tools are available if an A1C test is not accurate or sufficient?
Besides A1C tests, the most common measures of blood sugar are the oral glucose tolerance test (OGTT), CGM, and self-monitored blood glucose tests.
The OGTT is a diagnostic tool for diabetes and prediabetes that assesses a person’s response to consuming a fixed amount of sugar. Two hours after taking a sugar drink, blood sugar levels are measured.
Below 140 mg/dL is considered “normal,” between 140 mg/dL and 200 mg/dL points to prediabetes or impaired glucose tolerance, and above 200 mg/dL indicates diabetes. The OGTT is not useful for tracking diabetes management.
For people with diabetes, CGM has the advantage of monitoring blood sugar levels consistently throughout the day (every 5-15 minutes), which provides more detailed insights into time in range, low blood sugar, and hyperglycemia (high blood sugar).
If CGM is not available, taking frequent fingersticks with a blood glucose meter – when waking up, before and after meals, and before bed – can also indicate when blood sugar levels are going low, high, or staying in range.
What else can affect A1C?
While there are many unsuspecting things that can impact A1C, that doesn't invalidate the test results. Rather, knowing how certain factors can change A1C levels is a key part of using it as one measure of diabetes management. Here are some other non-glycemic factors that can affect A1C results.
Untreated anemia
Many of the conditions that affect A1C results are related to changes in the turnover of red blood cells, and thus notably, types of anemia. Untreated anemia can be caused by an iron or vitamin B12 deficiency.
Untreated anemia can misleadingly increase A1C values due to decreased production of red blood cells. To test for anemia, ask your healthcare provider about taking a complete blood count (CBC) test. Correction of anemia through treatment can also affect A1C results.
Asplenia (decreased spleen function)
The spleen is involved in the production and removal of red blood cells. Decreased spleen function may be caused by surgery, congenital disorders, and other blood disorders such as sickle cell disease. This may lead to misleadingly increased A1C. Asplenia can be identified by MRI, echocardiogram, chest X-ray, or a screening test.
Blood loss and blood transfusions
The body’s response to recent blood loss (creating more blood cells) or blood transfusion can misleadingly lower A1C, but the next A1C test should return to a more representative reading. Let your healthcare provider know if you have recently received a blood transfusion.
Cirrhosis of the liver
Cirrhosis refers to chronic liver damage that leads to scarring. Cirrhosis, in addition to affecting response to glucose-lowering medications (including insulin), may misleadingly lower A1C values. If you live with or are showing signs of liver damage, ask your healthcare provider about a liver examination.
Hemoglobinopathy and thalassemia
Hemoglobinopathy results in abnormal hemoglobin. Thalassemia refers to the lower production of functional hemoglobin. Depending on the abnormal form of the hemoglobin, hemoglobinopathy can result in either increased or decreased A1C values. Thalassemia can misleadingly lower A1C values due to the early destruction of red blood cells. Tell your healthcare provider if you have any known family members that have had thalassemia.
Hemolysis (rapid destruction of red blood cells)
Hemolysis is the rapid destruction of red blood cells, which may misleadingly lower A1C values due to the shortened red blood cell lifespan. This condition may be caused by an inappropriate immune response or artificial heart valves.
Untreated hypothyroidism
Hypothyroidism (low levels of thyroid hormone) may misleadingly increase A1C, while treatment with thyroid hormone can lower A1C. It's always a good idea to have your thyroid function measured during a routine blood test.
Pregnancy
Decreased red blood cell lifespan and an increase in red blood cell production may misleadingly lower A1C values in both early and late pregnancy. Ask about taking an oral glucose tolerance test, which is used to diagnose gestational diabetes. A common practice for pregnant people with diabetes is to use CGM.
Uremia
Uremia refers to high levels of waste normally filtered by kidneys in the blood. Untreated uremia may misleadingly increase A1C values. Dialysis is used to treat uremia – in this case, A1C is not a suitable test.
Medications
Certain medications that may misleadingly increase A1C include:
- Opioids (pain relievers): Duragesic (fentanyl), Norco/Vicodin (hydrocodone), Dilaudid (hydromorphone), Astramorph/Avinza (morphine), or OxyContin/Percocet (oxycodone)
- Long-term use of over 500 mg of aspirin per day
Medications that may misleadingly lower A1C include:
- Erythropoietin (EPO)
- Azcone (dapsone)
- Virazole/Rebetol/Copegus (ribavirin)
- HIV medications (NRTIs): Emtriva, Epivir, Retrovir, Videx-EC, Viread, Zerit, or Ziagen
Always discuss the appropriate use of opioids for pain and their possible effect on A1C as well. Tell your healthcare provider if you are taking any of these medications prior to your A1C test.
The bottom line
If you have diabetes, it’s also important to take the perspective that A1C is not a “grade” on diabetes management, but rather a helpful measurement tool that you and your healthcare providers can use to guide decisions and assess the risk of complications.
Credited: [Author: Jeemin Kwon], [Source: diaTribe Learn MAKING SENSE OF DIABETES | What's a 'Normal' A1C? When Is It Misleading?]
Healthy Bites















