Grains and diabetes prevention
Diets that include a high amount of whole grains can significantly decrease the risk of developing type 2 diabetes.
One study found that for 50 grams of whole grains consumed daily, there was a 23% reduced risk of diabetes. The researchers analyzed various studies involving whole grain consumption and found that 60 grams of whole grains was optimal for diabetes prevention.
How do whole grains prevent diabetes? Whole grain intake may reduce inflammation and postprandial blood glucose levels. Additionally, whole grain consumption can lower the risk of weight gain. All of these are factors in diabetes risk.
Grains and blood sugar management
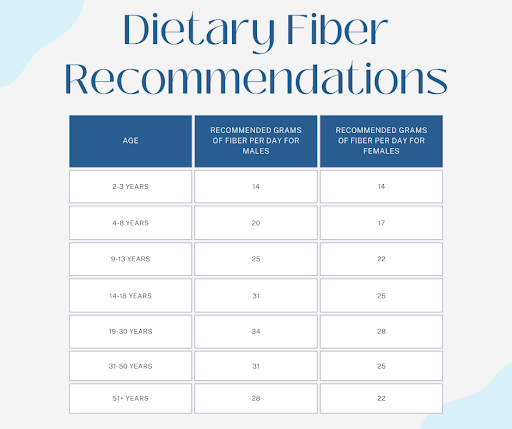
Already have diabetes? Grains should be a part of your diet. Upping your fiber intake to 35 grams per day (or increasing your intake by 15 grams) may lower your A1C, cholesterol, triglycerides, body weight, inflammation markers, and longevity.
Furthermore, grains have an impact on gut bacteria, thereby reducing inflammation, and repairing insulin signaling and beta cell dysfunction.
So what grains give you the best nutrient bang for your buck? Here are eight that will boost your fiber consumption – and taste great.
Best grains for people with diabetes
1. Farro
Nutrition in 1 cup cooked: 200 calories, 41 grams carbs, 4 grams fiber, 8 grams protein
Registered dietitian Christina Badaracco loves to recommend farro.
“It’s an ancient variety of wheat that includes three species: spelt, emmer, and einkorn. Its chewy texture and nutty flavor make it very satisfying,” Badaracco said. “Its versatility enables it to be incorporated into any meal of the day and dishes representing very diverse cultures.”
Ancient grains have a low glycemic index. When compared to other wheat products, farro has a higher protein, fat, and overall nutrient content. It can be added to soups or salads, used as a base in a grain bowl, or served as a side.
“It is a whole grain that provides many important vitamins, minerals, and polyphenols as well as fiber. When combined with produce, healthy fats, and protein, it can be an excellent component of a balanced meal that can help to manage blood sugar and weight,” Badaracco added.
2. Oats
Nutrition in 1 cup cooked: 166 calories, 28 grams carbs, 4 grams fiber, 6 grams protein
Oats are a popular grain and touted for their many health benefits.
“I suggest them because they're a good source of soluble fiber to help with blood sugar and lipid reduction. They are also filling, which may help with regulating appetite,” said registered dietitian Lisa Andrews.
The plant compounds in oats help to decrease post-meal glucose levels and boost healthy gut bacteria.
“In addition, they are affordable and easy to make in the microwave in two minutes. I like to add cinnamon and vanilla to mine as well as sliced almonds, chia seeds, or ground flaxseed,” Andrews said.
Beyond breakfast, oats make a terrific add-in to meatloaf and pumpkin oatmeal cookies.
3. Quinoa
Nutrition in 1 cup cooked: 222 calories, 39 grams carbs, 5 grams fiber, 8 grams protein
While most grains need complementary food to make a complete protein, quinoa is a stand-alone option. Quinoa is a powerhouse grain that is a complete protein and a remarkable source of fiber.
The protein peptides in quinoa have been found to help manage blood sugar by preventing your body from absorbing carbohydrates in the small intestine, thereby reducing glucose levels.
Quinoa is a wonderful staple for vegans and omnivores alike. Scramble cooked quinoa with eggs, use it to fill your tacos, or pair it with https://diatribe.org/roasted-tofu-and-brussels-sprouts-ginger-vinaigrettehttps://diatribe.org/roasted-tofu-and-brussels-sprouts-ginger-vinaigrette for a delicious dinner.
4. Sorghum
Nutrition in 1 cup cooked: 211 calories, 46 grams carbs, 4 grams fiber, 7 grams protein
A gluten-free option that contains plenty of antioxidants, sorghum is a cereal grain to add to your grocery list.
One study that evaluated the active compounds in sorghum identified 20 that work to promote overall health. Out of those, four seem to help with diabetes management by regulating a signaling pathway that affects energy use and metabolism.
Sorghum has a chewy texture, nutty flavor, and can be eaten in a variety of ways. This sorghum salad will help you reach your fiber goals. Additionally, sorghum can be popped for a crunchy snack.
5. Buckwheat
Nutrition in 1 cup cooked: 155 calories, 34 grams carbs, 4.5 grams fiber, 6 grams protein
Like quinoa, buckwheat contains all nine essential amino acids. Buckwheat is an excellent source of protein, fiber, and potassium. It’s also a gluten-free grain, making it an option for those with celiac disease.
One of the plant compounds in buckwheat, rutin, has been found to regulate gut bacteria and may slow digestion. Delayed absorption of carbohydrates may improve post-meal blood glucose spikes.
Buckwheat can be made into a porridge for breakfast or added to salads. You can also use buckwheat flour to make high-fiber pancakes and muffins.
6. Barley
Nutrition in 1 cup cooked: 193 calories, 44 grams carbs, 6 grams fiber, 4 grams protein
A cereal grain that is a staple worldwide, barley is a slowly digested starch.
“Barley is a great whole grain for its versatility and nutrition. Barley is a great source of protein as well as iron and magnesium,” said registered dietitian Amanda Lane.
Barley and barley flour have a lower glycemic index than wheat and may play a role in regulating gut bacteria. It also has a positive impact on gut hormones and appetite.
Barley pairs well with most savory dishes and can also be eaten as a porridge or sweetened with fruit for a different twist on this adaptable grain.
7. Wheat
Nutrition in 1 cup cooked bulgur: 152 calories, 34 grams carbs, 8 grams fiber, 6 grams protein
Nutrition in 1 slice whole wheat bread: 70 calories, 12 grams carbs, 3 grams fiber, 4 grams protein
Wheat is probably the most well-known grain. While wheat has been vilified by some, it can be an inexpensive way to up your fiber intake. Of course, it should be avoided by those who have a gluten sensitivity. But most people tolerate wheat just fine.
The key is to choose whole wheat products that leave the wheat kernel intact. Opt for whole grain bread for your sandwiches and whole wheat flour for baking. The germ and bran (which are often removed in processed, white flour foods) are healthier than processed wheat.
Wheat germ has also been found to reduce stress and depression scores in people with diabetes by positively impacting a protein that promotes nerve growth and connection.
Bulgur, a hulled wheat kernel product, has a high fiber and manganese content and is another way to incorporate whole wheat into your diet.
8. Amaranth
Nutrition in 1 cup cooked: 250 calories, 46 grams carbs, 5 grams fiber, 9 grams protein
A pseudocereal like quinoa and buckwheat, amaranth is a gluten-free grain that is rich in nutrients. Amaranth has a higher protein content than cereal grains and is rich in calcium, potassium, and magnesium.
It’s also worth adding to your diet because of its antioxidant and peptide activity, which can promote health and regulate blood sugar. Try amaranth flour in your baked goods or pizza dough for a heart-healthy alternative to processed flour.
Amaranth can also be made into a porridge or a nutty-tasting side dish. It can also be popped for a snack or crunchy topping for your salad.
In summary, we all need to prioritize fiber for optimal digestion and health. Incorporating a variety of whole grains, rather than processed foods, is an excellent strategy to meet your fiber targets each day.
Learn more about what to eat with diabetes here: