Many people with diabetes – even those using the latest technology – struggle with high blood sugar after eating. We spoke with experts for tips on how to minimize those stubborn glucose spikes.
We’ve all been there: it’s been a long, demanding day at work and you’re excited to sit down for dinner at your favorite restaurant.
Or maybe you’re eager to watch the game and dig into a feast of wings, nachos, and sliders with friends and family. Perhaps you’ve been traveling or on your feet all day and are ready to gobble up the first food you encounter.
Regardless of the situation, it’s likely you don’t want to take the time to bolus and wait for your insulin to kick in before you start eating. After all, meals are often a social activity, and it’s no fun to wait while others are chowing down.
But as the meal wears on, you catch a glimpse of your phone and are startled to see your blood sugar is well into the 200s and rising. Soon, you start to recognize the telltale signs of high blood sugar: anger, frustration, fatigue, blurred vision, and a general feeling of unease.
There’s no doubt about it – navigating meals can be tricky when you have diabetes. Even among people who use automated insulin delivery (AID) systems, research suggests that achieving postprandial glycemic control can be difficult.
Why do blood sugar spikes after meals happen?
Sudden increases in blood glucose after eating are normal, even in people without diabetes. After consuming carbohydrates, blood sugar levels rise as our bodies break carbohydrates down into sugars.
In people without diabetes, this increase in blood sugar triggers the immediate release of insulin. Within minutes, insulin starts transporting glucose from the bloodstream into cells, helping to reduce blood sugar after eating. Post-meal blood glucose spikes are usually temporary and often go unnoticed in those without diabetes.
However, in people with diabetes, blood sugar spikes can be more pronounced and last longer. Insulin delivered via injections or an insulin pump takes longer to start working compared to the insulin produced naturally by the body, meaning blood glucose will continue to rise while the injected insulin kicks in.
People with diabetes have other hormonal differences that can affect the speed of digestion. Those without functional beta cells also cannot produce the hormone amylin, which helps slow digestion and reduces post-meal glucose. That means people without enough amylin may experience challenges with high glucose levels after eating.
If you’ve been struggling with post-meal hyperglycemia, take stock of your current circumstances and if you’ve experienced major life changes recently, suggested LaurieAnn Scher, certified diabetes care and education specialist.
Have you experienced stressors, such as studying for a big exam, switching jobs, or moving? This can trigger the release of stress hormones like cortisol, which can promote weight gain and affect metabolism, including insulin resistance.
Maybe your eating or exercise patterns have shifted, perhaps due to changes like starting college, moving in with a partner, or navigating parenthood. Diet changes can lead people to gain more muscle or fat. With a different proportion of fat and muscle mass, insulin resistance can fluctuate, impacting your insulin needs, Scher added.
Many other factors can affect insulin resistance and blood glucose management, such as using birth control, environmental conditions, dehydration, and more.
Why is it important to reduce blood sugar spikes?
High blood sugar after meals raises your risk of diabetes complications, including kidney disease, cardiovascular disease, and diabetic neuropathy. Post-meal hyperglycemia can also affect quality of life, leading to negative effects on mood, diabetes distress, and issues like brain fog or sluggishness.
To put it simply, high blood sugar after eating “doesn’t feel great, and it can be hard to think and see,” said Scher.
Research also suggests that better glycemic control after meals is linked to improved A1C and fasting glucose levels.
According to the American Diabetes Association 2024 Standards of Care, you should aim for blood sugar to be less than 180 mg/dL within 1-2 hours after you start eating. By contrast, in most people without diabetes, two-hour postprandial blood sugar levels are typically less than 120 mg/dL and rarely exceed 140 mg/dL.
How to prevent blood sugar spikes after eating
From medications to diet and physical activity, there are many different strategies to prevent bothersome blood sugar spikes after meals. As with all parts of diabetes care, it’s important to recognize that what works for one person may not work for someone else.
“It’s all about tailoring to the patient’s needs, comfort level, background, what they’ve tried, and what they’re willing and interested in,” said Rina Hisamatsu, a registered dietitian at the Michigan Collaborative for Type 2 Diabetes (MCT2D).
1. Experiment with different insulins and dose timing
For any diabetes medication, Scher advised, “Don’t set it and forget it.”
That is, you should regularly examine basal and bolus insulin, along with your other medications. You may need to adjust your insulin regimen and tweak bolus doses and timing throughout your life.
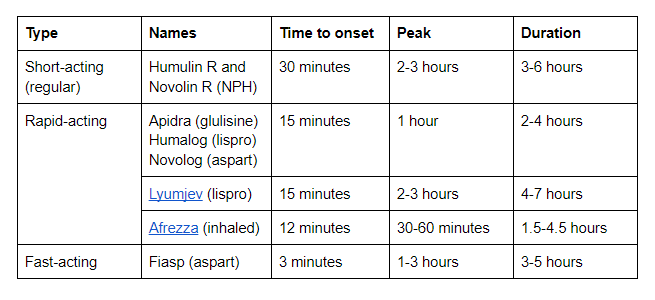
There are several different types of mealtime insulin, each with its own time to onset of blood glucose lowering:
4. Offset carbs with fat and protein
Understanding the different types of carbohydrates is key to managing post-meal blood sugar spikes.
“I’ve always said there’s nothing that a person with diabetes can’t eat, except poison and food with poison,” Scher said. “You can have cake, candy, etc. You’re human. You just need to learn how to manage it.”
Carbohydrates can be divided into two general categories:
- Simple carbs are sugars. These carbs are broken down quickly and usually lead to big spikes in blood sugar. Examples include soda, baked goods, breakfast cereals, and fruit juice.
- Complex carbs are broken down more slowly and lead to more predictable, gradual increases in blood sugar. Examples include beans, fruits, vegetables, and whole grains.
Hisamatsu suggested starting with “low-hanging fruit” by identifying parts of your diet where you tend to eat more refined or simple carbohydrates. Maybe you’re flying out the door to work in the morning, so breakfast has become a sugary granola bar. Or you crave fruit juice at lunch and a cookie for dessert.
Once you’ve identified those areas, consider ways to add more complex carbs and fiber-rich foods. Start with small modifications and try habit stacking to ensure sustainable changes.
Overall, Hinamatsu recommended focusing on increasing fiber and protein intake, while adding fat for flavor and fullness.
“When people are less focused on carb intake, we have seen that it can improve their postprandial glucose,” she said.
5. Try setting a temporary basal rate
In the same way that some people choose to lower their basal insulin rate during exercise, you could consider temporarily increasing your basal rate by a certain percentage before or after meals.
Likewise, some insulin pumps allow you to set a lower pre-meal target, such as 80 or 85 mg/dL rather than 95 mg/dL before eating.
Setting a temporary basal rate can be helpful when you’re eating food that has significant refined carbohydrates in it, such as pastries, bread, pasta, pancakes, pizza, and even white rice. This strategy may be especially beneficial for those with more insulin resistance.
You might have to experiment through trial and error to figure out what works best for you. Consult your healthcare provider to find the ideal basal rate for mealtimes.
6. Use CGM as a tool to inform decisions
Continuous glucose monitors (CGM) provide valuable information that can help you manage post-meal blood sugar.