6 Things to Know About Wearing a Continuous Glucose Monitor
Continuous glucose monitoring (CGM) can dramatically improve glucose management – but these devices can also bring their own set of challenges, especially if you have sensitive skin. Luckily, there are several products to help you make insertion easier.
If you’ve ever experienced skin irritation when wearing a continuous glucose monitor (CGM), you’re not alone. From a minor rash to a painful allergic reaction, skin problems are no fun – they can negatively impact quality of life or even lead to device discontinuation. In a recent study, about one in four CGM users reported skin reactions, and about 3% stopped wearing their sensor due to reactions.
However, there are several products designed to make these devices more comfortable and effective. Plus, CGM companies are continually innovating their sensors and adhesives to make them more comfortable, accurate, and longer-lasting.

Who is at risk for skin irritation?
People use CGM in different ways and for different reasons. Those with insulin-dependent diabetes typically use CGM every day, while people with less severe diabetes may use CGM a few times a year to support healthy lifestyle choices.
Sarah Hormachea, a registered dietitian and Certified Diabetes Care and Education Specialist (CDCES), noted that intermittent users tend to have fewer skin-related issues since they have less exposure to the sensors, adhesives, and years of insulin injections. If you use CGM intermittently, you may have more flexibility in the selection of your CGM insertion site, Hormachea said. Meanwhile, if you use CGM every day for many years of your life, it’s a good idea to be more prudent with insertion, rotation, and removal.
People with sensitive skin, a history of eczema, or other skin barrier conditions may also be at a higher risk of developing a contact rash. Likewise, research suggests people who use both CGM and insulin pumps are more likely to report irritation, compared to those who only use pumps.
Expert tips to avoid skin irritation when wearing a CGM
While proper CGM insertion can seem overwhelming at first – so many steps and details to keep track of! – there are several tips to make the process smoother.
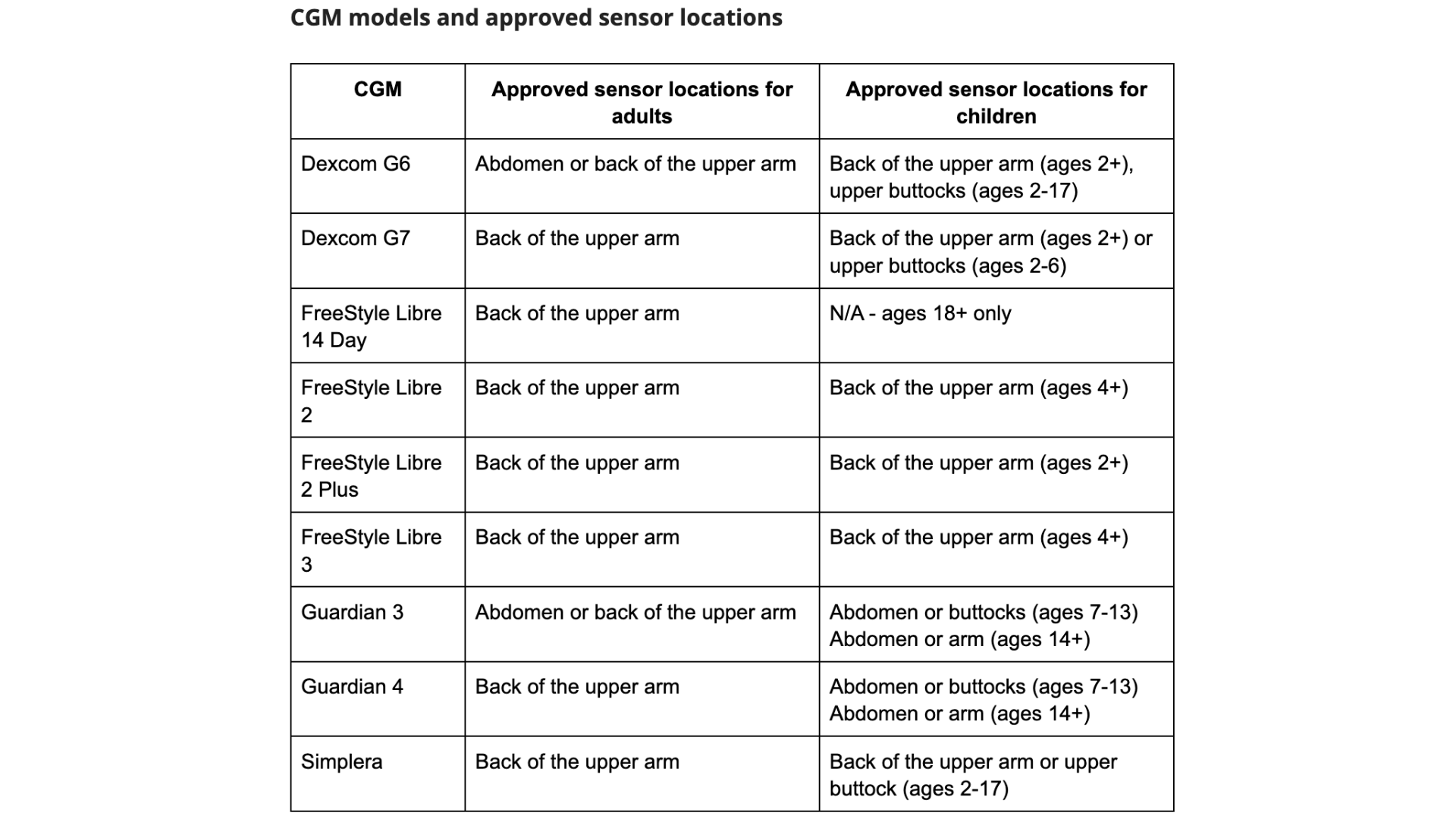
1. Choose the right sensor site
There are many different CGM models, each with pros and cons – including where they can be worn. You might need to do some trial and error to find the best sensor site for you.
Once you’ve determined where on your body to place the device, look for the following characteristics for a sensor site. An area:
- At least 3 inches away from your insulin pump or injection site
- Away from bones, irritation (like stretch marks or eczema), waistbands, scars, and tattoos
- Unlikely to be bumped or laid on while asleep
- With enough “padding” or fat
Hormachea noted that people who have experienced a lot of weight loss sometimes have a hard time finding CGM sites. Skin elasticity can decrease after weight loss, making the skin less firm and preventing devices from sticking.
While each CGM model is approved for specific application sites, Hormachea said in reality, she has seen sensors worn in many different places. People who have been wearing CGM for many years may start to run out of space; they may need to pick a more unusual place, such as the lower back, hips, or thighs.
Some people find it difficult to insert a new sensor into the back of the arm by themselves. If that’s the case, they should ask a trusted caregiver, family member, or friend for help
2. Hygiene is key
3. Prevent contact rashes
If you’re prone to irritation, some healthcare providers recommend using a nasal spray like Flonase, which is a topical steroid that helps calm the skin. Bellini suggested spraying your CGM site a couple of times to create a contact barrier, which can prevent rashes. You can buy the generic version over-the-counter for about $25.
You can also consider creating a physical barrier using a product like the sticky patch TegadermHP, which blocks liquids, viruses, bacteria, and other contaminants from touching the skin. Bellini suggested applying TegadermHP and then placing the sensor through the dressing – that way, the sensor won’t touch your skin directly. A box of 100 dressings costs about $60.
Many who belong to online diabetes communities have felt more at ease knowing they aren’t alone in having skin reactions to wearing a CGM. Susannah Chen, a managing editor at diaTribe who uses the Dexcom G6, experienced a number of skin reactions when starting on CGM with an AID system, even after speaking with her endocrinologist and dermatologist. She ultimately found the most helpful advice in a Facebook group for adults and caretakers of children with type 1 diabetes.
“Some people suggested ‘off-gassing’ the sensor, or unpeeling the backing paper off the sensor and letting the adhesive side air out for 24 hours in advance of applying it to the skin,” Chen said. “I personally found that to be really beneficial.”
4. Consider extra adhesives
Some people have a hard time keeping their CGM in place for the full one to two weeks. Humid weather, intense physical activity, or even bumping your sensor while getting dressed can all cause devices to fall off.
If you’re prone to losing sensors, Hormachea suggested first re-evaluating your device placement. Is your CGM on a body part that’s often being stretched or bumped? Do you tend to sweat a lot in that area? If so, consider switching your sensor site.
For instance, the flank (the areas on the sides of the abdomen) are a popular sensor site for Dexcom G6 users. However, if you're a frequent side sleeper, you may want to avoid those areas as they could result in compression lows.
There are also different types of products that can help keep your CGM in place:
- Wipes or sprays that make your skin extra sticky, like Skin Tac or Skin-Prep
- Overlay patches that provide extra protection (many come in fun colors and designs!)
- Holsters or harnesses that consist of a stretchy band and a plastic cap that covers the sensor
Check out our Skingrip products:
https://www.diabeticsupplieinc.com/store
5. Rotate, rotate, rotate
It’s important to give your skin time to heal when using a CGM, insulin pump, or injections. Rotating between different sites can help improve the CGM’s accuracy and reduce your risk of skin irritation or problems.
There are several different strategies to help you track and rotate your CGM:
- Imagine a clock at the sensor site. Start by placing the device in the 12 o’clock position, then switch to 3 o’clock, 6 o’clock, and so on.
- Visualize the letter M or W and use each point of the letter as an insertion point.
- Map out a grid pattern (2x2, 3x3, and 4x4 work well) onto the body part where you place your sensor. Start with one quadrant of the grid and gradually rotate your sensor through all the possible boxes.

6. Take care when removing your sensor
Hormachea recommended removing a CGM like a Band-Aid. “Use one hand as support and the second hand to peel the sensor away from the skin in one motion,” she said.
If you’re having a hard time removing your sensor, consider using a product to loosen the adhesive. Medical grade wipes (like Uni-Solve) can help soften residue from the adhesive. You can also use baby oil or any other oily product (such as micellar water) to loosen the adhesive.
The bottom line
CGMs are a powerful tool for diabetes management that have been shown to increase time in range, reduce hypoglycemia, and improve quality of life. As with all parts of diabetes care, you may need to experiment with trial and error to find the sensor location, rotation pattern, and adhesive products that work best for you.
If you continue to struggle with wearing a CGM, contact your healthcare provider or CDCES for more support – they are a valuable resource for any questions you might have about diabetes technology or medications.
“A CDCES or diabetes-trained dietitian or nurse can often look at someone right away and say ‘let’s try this,’ and give you customized pointers,” Hormachea said. “Meeting with a professional can really enhance your CGM experience.”
Credited: [Author: April Hopcroft], [Source: diaTribe Learn MAKING SENSE OF DIABETES | 6 Things to Know About Wearing a Continuous Glucose Monitor]
Healthy Bites